
Pharmacy Times offers relevant, clinical information for pharmacists that they can use in their daily practice. These include OTC and Rx product news, disease conditions, patient education guides, drug diversion and abuse, and more.
Issue link: http://pharmacytimes.epubxp.com/i/312123
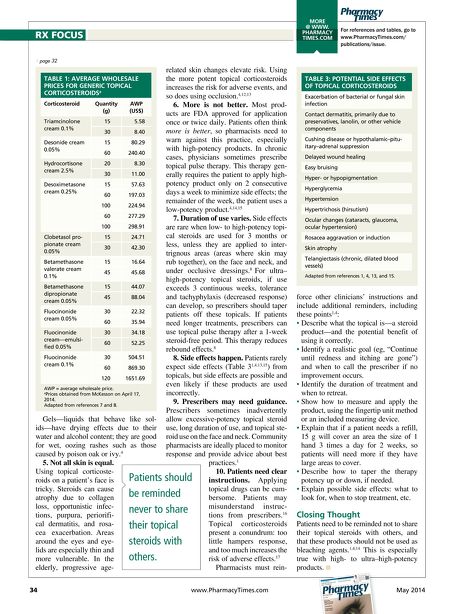
For references and tables, go to www.PharmacyTimes.com/ publications/issue. MORE @ WWW. PHARMACY TIMES.COM Gels—liquids that behave like sol- ids—have drying effects due to their water and alcohol content; they are good for wet, oozing rashes such as those caused by poison oak or ivy. 4 5. Not all skin is equal. Using topical corticoste- roids on a patient's face is tricky. Steroids can cause atrophy due to collagen loss, opportunistic infec- tions, purpura, periorifi- cal dermatitis, and rosa- cea exacerbation. Areas around the eyes and eye- lids are especially thin and more vulnerable. In the elderly, progressive age- related skin changes elevate risk. Using the more potent topical corticosteroids increases the risk for adverse events, and so does using occlusion. 4,12,13 6. More is not better. Most prod- ucts are FDA approved for application once or twice daily. Patients often think more is better, so pharmacists need to warn against this practice, especially with high-potency products. In chronic cases, physicians sometimes prescribe topical pulse therapy. This therapy gen- erally requires the patient to apply high- potency product only on 2 consecutive days a week to minimize side effects; the remainder of the week, the patient uses a low-potency product. 4,14,15 7. Duration of use varies. Side effects are rare when low- to high-potency topi- cal steroids are used for 3 months or less, unless they are applied to inter- trignous areas (areas where skin may rub together), on the face and neck, and under occlusive dressings. 8 For ultra– high-potency topical steroids, if use exceeds 3 continuous weeks, tolerance and tachyphylaxis (decreased response) can develop, so prescribers should taper patients off these topicals. If patients need longer treatments, prescribers can use topical pulse therapy after a 1-week steroid-free period. This therapy reduces rebound effects. 8 8. Side effects happen. Patients rarely expect side effects (Table 3 1,4,13,15 ) from topicals, but side effects are possible and even likely if these products are used incorrectly. 9. Prescribers may need guidance. Prescribers sometimes inadvertently allow excessive-potency topical steroid use, long duration of use, and topical ste- roid use on the face and neck. Community pharmacists are ideally placed to monitor response and provide advice about best practices. 1 10. Patients need clear instructions. Applying topical drugs can be cum- bersome. Patients may misunderstand instruc- tions from prescribers. 16 Topical corticosteroids present a conundrum: too little hampers response, and too much increases the risk of adverse effects. 17 Pharmacists must rein- force other clinicians' instructions and include additional reminders, including these points 1,4 : • Describe what the topical is—a steroid product—and the potential benefit of using it correctly. • Identify a realistic goal (eg, "Continue until redness and itching are gone") and when to call the prescriber if no improvement occurs. • Identify the duration of treatment and when to retreat. • Show how to measure and apply the product, using the fingertip unit method or an included measuring device. • Explain that if a patient needs a refill, 15 g will cover an area the size of 1 hand 3 times a day for 2 weeks, so patients will need more if they have large areas to cover. • Describe how to taper the therapy potency up or down, if needed. • Explain possible side effects: what to look for, when to stop treatment, etc. Closing Thought Patients need to be reminded not to share their topical steroids with others, and that these products should not be used as bleaching agents. 1,4,14 This is especially true with high- to ultra–high-potency products. n 34 www.PharmacyTimes.com May 2014 Patients should be reminded never to share their topical steroids with others. page 32 RX FOCUS TABLE 1: AVERAGE WHOLESALE PRICES FOR GENERIC TOPICAL CORTICOSTEROIDS a Corticosteroid Quantity (g) AWP (US$) Triamcinolone cream 0.1% 15 5.58 30 8.40 Desonide cream 0.05% 15 80.29 60 240.40 Hydrocortisone cream 2.5% 20 8.30 30 11.00 Desoximetasone cream 0.25% 15 57.63 60 197.03 100 224.94 60 277.29 100 298.91 Clobetasol pro- pionate cream 0.05% 15 24.71 30 42.30 Betamethasone valerate cream 0.1% 15 16.64 45 45.68 Betamethasone dipropionate cream 0.05% 15 44.07 45 88.04 Fluocinonide cream 0.05% 30 22.32 60 35.94 Fluocinonide cream—emulsi- fied 0.05% 30 34.18 60 52.25 Fluocinonide cream 0.1% 30 504.51 60 869.30 120 1651.69 AWP = average wholesale price. a Prices obtained from McKesson on April 17, 2014. Adapted from references 7 and 8. TABLE 3: POTENTIAL SIDE EFFECTS OF TOPICAL CORTICOSTEROIDS Exacerbation of bacterial or fungal skin infection Contact dermatitis, primarily due to preservatives, lanolin, or other vehicle components Cushing disease or hypothalamic–pitu- itary–adrenal suppression Delayed wound healing Easy bruising Hyper- or hypopigmentation Hyperglycemia Hypertension Hypertrichosis (hirsutism) Ocular changes (cataracts, glaucoma, ocular hypertension) Rosacea aggravation or induction Skin atrophy Telangiectasis (chronic, dilated blood vessels) Adapted from references 1, 4, 13, and 15. Pg 32 PT_0514_RxFeature.indd 34 5/7/14 5:25 PM